As an Orthopaedic Surgeon I have treated many athletes who train in BJJ, and from other sporting disciplines including Muay Thai, football, rugby and basketball with ACL tears. I’m also a Blue Belt at Evolve MMA in Singapore. This articles serves to share some of my knowledge and experience in dealing with ACL injuries to inform a better understanding of this common condition within the BJJ community. Most sporting activities have some risk of injury. The good news is that compared to many other sports like football or basketball, BJJ is relatively safe when it comes to ACL injury.
What is an ACL tear?
ACL stands for the Anterior Cruciate Ligament. It is one of the main ligaments (tough rope like structure) in the knee. The ACL sits in the middle of the knee and attaches the femur (thigh bone) to the tibia (shin bone). It stops the tibia from sliding forward and rotating excessively. If your ACL is torn then your knee may buckle and give way during a pivoting movement / sudden change of direction.
Healthy and stable ACL
How do ACL tears occur?
ACL tears typically occur when the foot is planted and knee rotation occurs (e.g. during a hip throw). If during knee rotation the knee collapses inwards (called a valgus or ‘knock kneed’ movement), then this may place enough stress on the ACL to cause a tear. Another mechanism that cause an ACL tear is hyper-extension (over-straightening) of the knee which can occur from a direct blow to the front of the knee. Commonly ACL tears occur without any contact with other athletes, but in BJJ we are also at risk of our partners applying additional force to our knees at all angles e.g. during double leg take downs, heel hooks and knee bars, or falling on top of us when we try to throw them.
Unfortunately for female Ju-jiteiros, you are at greater risk for an ACL tear than guys.1 The exact reason is unknown but is thought to include differences in alignment, size and mechanics of your knees.2
How do I reduce the risk of an ACL tear?
1. Avoid Ego. If you are in a leg lock and feel your knee is being twisted to shreds, please tap out. Likewise don’t hurt your training partner and be ‘that guy’ who trains like every situation is a world championship final.
2. Listen carefully to your teacher (or instructor) to learn correct technique, specific details, and minimum amount of force required.
3. Warm up before every training session, cool down and stretch your hamstrings and quads afterwards – not always easy I know when you are rushing off to work after your morning/lunchtime training session.
4. Strengthening and balance – Try doing a single leg squat on each leg. If you are unable to squat without your knees wobbling and turning to point inwards then you may need to see a physiotherapist or strength conditioner to work on strength training (particularly of your quads and hamstrings), core and hip strength, and balance.
5. Enroll in an ACL injury prevention program – not everyone is fortunate enough to live in an area where such programs exist. Typical programs focus on;
a) Plyometrics or jumping exercises in which muscles exert maximum force in short intervals of time, with the goal of increasing power – however there has to be sufficient emphasis on proper technique and body mechanics;
b) Neuromuscular training which aims to improve muscle firing patterns, increase dynamic joint stability, and ability to perform movement patterns and skills. This may include balance exercises, wobble boards, single-leg stability activities, agility drills, and sport-specific exercises;
c) Strength training – usually most effective when combined with plyometrics and neuromuscular training.3
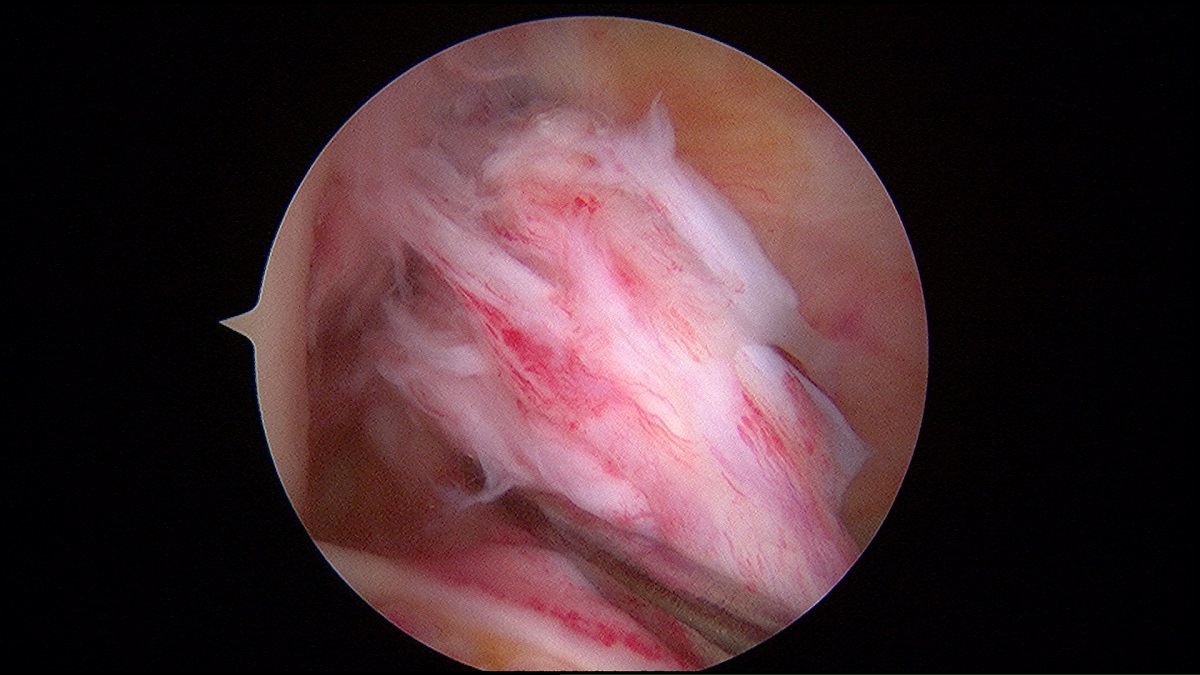
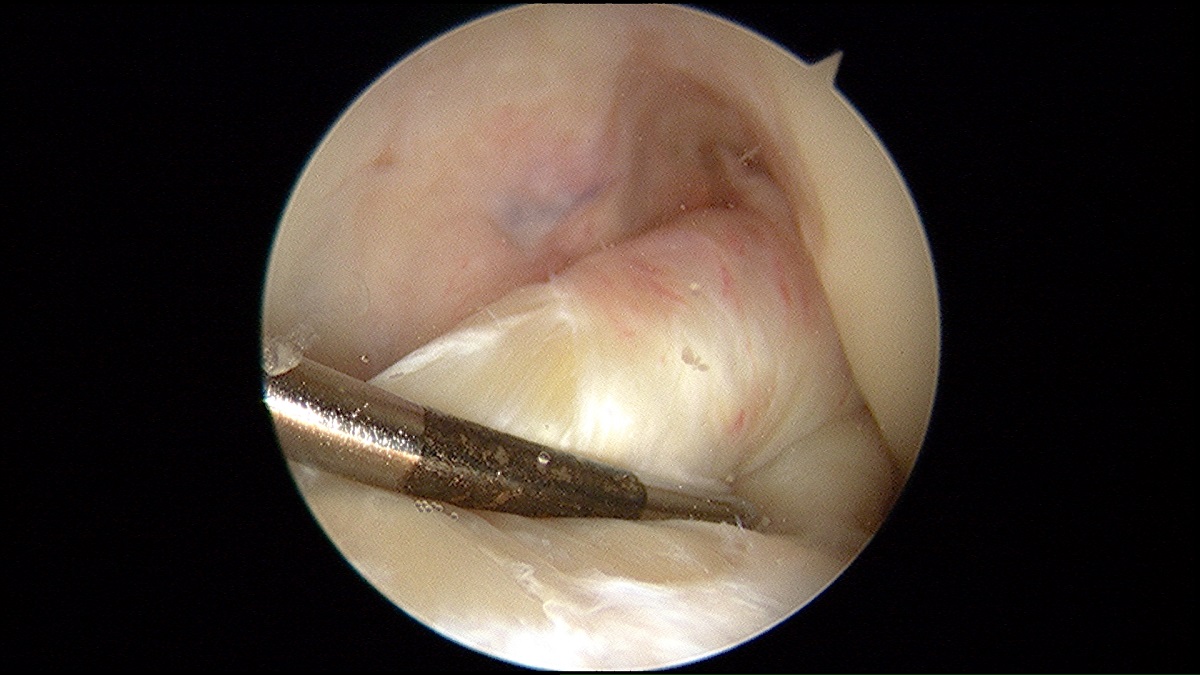
Torn unstable ACL
How do I know I have an ACL tear?
Athletes who tear their ACL often feel a ‘pop’ and their knee may swell suddenly (as the torn ligament bleeds). A key feature is that they are unable to walk or continue training due to pain. When the knee swelling eventually subsides their knee may feel unstable or even give way. If that wasn’t bad enough, up to half of ACL injuries occur with injuries to other ligaments, cartilage or meniscus (shock absorbing fibrous disc) in the knee which may cause additional pain, instability and locking (knee cannot fully straighten).
Positive Lachman’s test for torn ACL
What should I do next?
RICE. Stop training immediately and apply ice. You can pick up a knee support or brace from most pharmacies. Rest and put your leg up to reduce swelling. Anti-inflammatories can help. If you are lucky enough to have a physiotherapist or orthopaedic surgeon training at your gym then ask their advice. If the problem persists past a few days then I would strongly suggest seeing a specialist. It’s an added bonus if they actually train in BJJ. Your specialist should ask you a lot of questions about how exactly the injury occurred and carefully examine the knee to make the diagnosis of an ACL tear. If they don’t bother to physically examine you then I strongly suggest the seeking of a second opinion.
Imaging in the form of an MRI scan is usually the next step. X-rays are cheaper and faster to perform than MRIs and can show fractures, degenerative change and subtle signs of ACL injury (such as the ‘Segond fracture’) but in general are less helpful than MRI scans for diagnosis of ACL tear. I’m very blessed in Singapore that I can arrange an MRI scan of the knee almost immediately, but in other parts of the world you may have to wait a long time. During my training as a Surgeon in the UK, public system patients would typically queue 18 months following injury to see a specialist, and then wait another 3-6 months for their MRI scan.
Famous martial artists who have suffered an ACL tear include George St Pierre, Ronda Rousey, Conor McGregor, Tito Ortiz, Vitor Belfort, Ken Shamrock, Dan Henderson, the list goes on. So if you have an ACL tear then you are in excellent company, and the good news is that all these athletes were able to resume their careers after an ACL reconstruction.
Can the torn ACL heal on its own?
The completely torn ACL usually does not heal well on its own because it is in an environment which does not allow good healing. Normally ligaments heal by forming a blood clot. The ACL is within the knee joint itself, and continuously bathed by synovial fluid which is thought to prevent clot formation.4 I also liken an ACL to a rope, and if completely torn in the middle, it is difficult for the rope ends to come together to heal, particularly as the knee is moving all the time. However some athletes are able to return to BJJ if they have a partial ACL tear, minimal instability or are able to adapt their game to an unstable knee.
Torn unstable ACL
Is ACL reconstruction surgery my only treatment option?
ACL reconstruction is when the torn ACL is completely replaced by a tissue “graft” (usually made of hamstring tendons which sit behind the inner thigh) to provide stability to the knee. It is the recommended treatment option for athletes who have knee instability following an ACL tear, and are unable to play sports.
It is worth seeing a good physiotherapist on the recommendation of your surgeon, and undergo rehab before considering surgery. This allows your knee to regain full range of movement and strength, as well as allow bone bruising to settle. Some doctors have also argued that ACL reconstruction is associated with a lower risk of early arthritis (degenerative change) on Xray.6
ACL repair is a newer treatment suitable for certain types of tears where the ends of the torn ACL are reattached to the thigh bone using a device called an internal brace. Most ACL tears are not suitable for direct repair and there can be a high rate of revision surgery with repair (1 in 8 patients in some papers). There are many studies, particularly on animals, on the use of stem cell and platelet rich plasma in ACL healing, but these technologies are still in an experimental stage and the “gold standard” treatment is still ACL reconstruction surgery.5

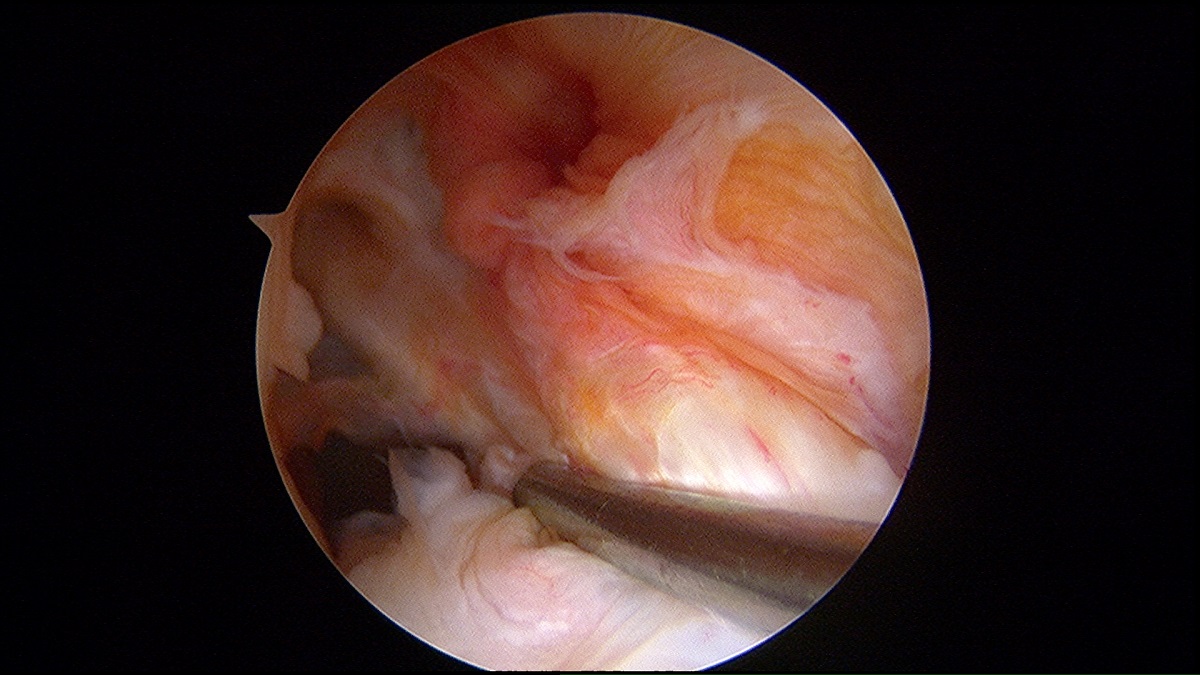
Femoral tunnel for ACL graft
Who can benefit most from an ACL reconstruction surgery?
I recommend ACL reconstruction for patients with knee instability and:
Active adult patients involved in sports requiring pivoting or turning such as BJJ/MMA/Muay Thai.
Active adult patients with jobs, particularly heavy labour, requiring pivoting or turning
Older patients (e.g. above 50) who compete at an elite level and do not have degenerative change in their knees
Children or adolescents with ACL tears – a modified technique can be used to reduce risk of injury to the growth plate.
Athletes with other injuries to their knees as well as ACL tear –ligaments such as the PCL (posterior cruciate ligament) LCL (lateral collateral ligament), menisci and cartilage. Particularly for some meniscus tears, a better result can be had if the repair is done at the same time as an ACL reconstruction.
What are the different types of ACL reconstruction surgeries?
A) Types of ‘Graft’ in ACL surgery:
All reconstruction surgeries use a ‘graft’ or transplanted tissue, to replace the torn ACL.
These grafts include:
1. Hamstrings tendons – the patient’s own tendons (“autograft”) are harvested from the inside of the knee during surgery using a small incision. Alternatively donated tendon can be used to replace your torn ACL (allograft). Athletes who have very flexible joints (hyperlaxity), a very loose MCL (medial collateral ligament) or very small hamstring tendons may be more suitable for allograft (donated tendon from a cadaver) or patellar tendon graft (below).
2. Patellar tendon – The middle third of the patellar tendon of the patient, along with a bone plug from the shin and the kneecap is harvested. It is effective as the hamstring tendon graft but has a higher risk of kneecap pain, particularly when kneeling, and fracture of the kneecap itself. There is usually a larger scar on the front of the knee.
3. Allograft – sterilised donated tissue from a cadaver (dead person) which doesn’t sound appealing, but can be less painful than having your own hamstrings harvested and can be useful for many different reasons – best to discuss carefully with your surgeon.
B) Different Surgical Techniques in ACL Reconstruction:
1. Medial portal vs Transtibial
When ACL reconstruction first began, surgeons drilled their bone tunnels in a straight line from the shinbone into the thighbone (transtibial). This results in a bone tunnel in the thighbone which is not where the original ACL used to sit. In contrast using the medial portal technique, surgeons place the bone tunnels and graft as close to the original position of the ACL as possible (anatomical position). Some surgeons believe that using a transtibial technique can result in greater rotational instability of the knee and a higher revision rate.7
2. All-inside / Graftlink Technique
The all-inside technique uses reverse drilling to reduce the amount of bone removed from the knee. It also needs only one hamstring to recreate the ACL graft. The rationale is that this technique may be more minimally invasive and less painful than conventional methods.8
3. Single bundle versus double bundle
Some surgeons try and recreate the two main bundles of the ACL by drilling 4 holes in the bones of your knee instead of 2 and using two separate grafts. There is no major difference in results between single or double bundle ACL reconstruction – you can achieve an excellent result with either technique.9
4. Growth plate preserving
Young children or adolescents with ACL injury may still have open growth plates (where new bone is laid down and allows limbs to get longer). These fuse around age 14 in girls, and age 16 in boys. Using a standard technique for ACL reconstruction (transphyseal) may injure the growth plates and stop the bones from growing (growth arrest). Your surgeon should screen for growth plates and either wait until your child has stopped growing, or use a special technique to avoid the growth plate (Epiphyseal or extraphyseal).
When is the best time to go for an ACL reconstruction surgery after an injury?
Within a few weeks to months of injury is ideal.10 Delaying surgery for more than 6 months is associated with a higher risk of injury to other structures in the knee like cartilage and menisci.11,12 Ideally you will have undergone physiotherapy to reduce swelling, regain full range of movement and strengthen your quadriceps (front thigh muscles) before the operation.
ACL reconstructed using hamstring graft
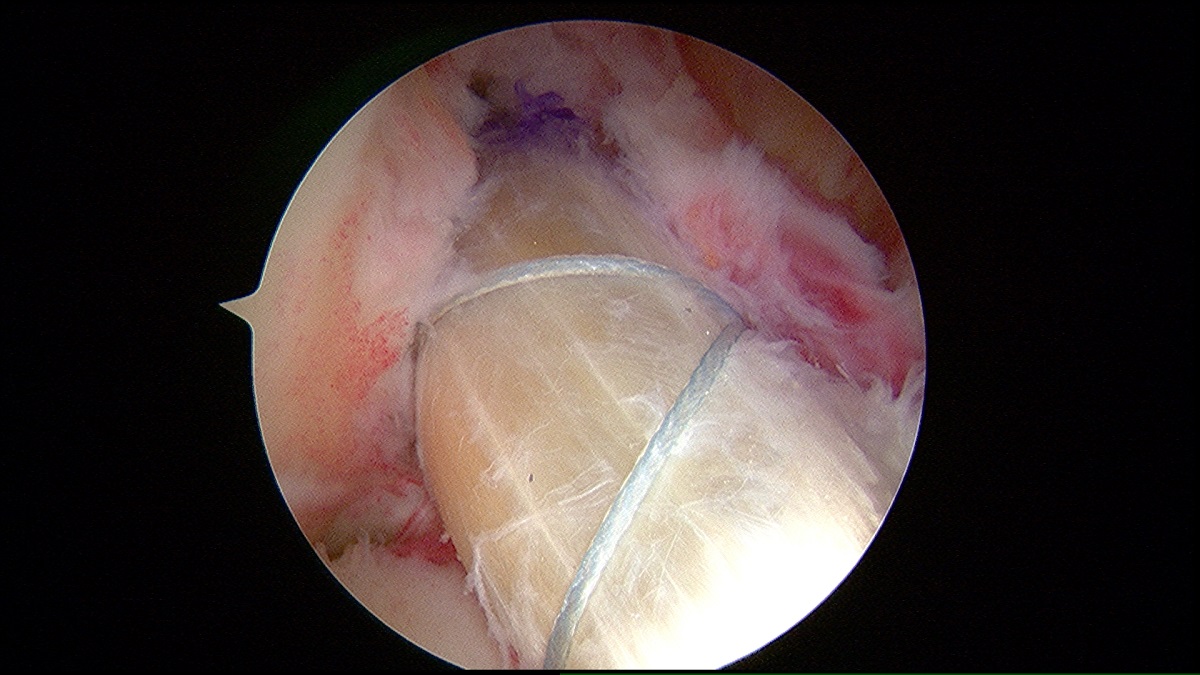
What happens during an ACL reconstruction surgery?
• You will have an anesthetic and typically be ‘asleep’ during surgery.
• Two small keyhole incisions are made at the front of the knee. Other incisions are made to harvest the hamstring or patellar tendon graft.
• The knee is thoroughly inspected with a camera (arthroscope), and small tunnels are drilled in the femur and tibia where the ACL normally sits.
• The correct placement of these tunnels is important to achieve a good result
• The graft is passed through the tunnels and secured with a metal or plastic buttons and screws.
• The whole procedure takes around an hour.
• You will be able to walk the same day after surgery with crutches.
• In the UK and Australia where I trained, most patients can go home on the same day of surgery.
What is the recovery process like after an ACL reconstruction surgery?
• After the surgery the knee is sore, but you’ll be given some strong painkillers.
• You’ll be able to get up and walk straight after the surgery, with crutches
• Some patients are well enough to go home the same day
• It’s important to start physiotherapy soon after the operation
• You may be on crutches for up to six weeks
• You can return to office based work after 2 weeks.
• If you have a physically demanding job it will take longer before you can return
• Return to sports can be anything from 6-12 months, usually 9 months
Some people recover quickly, some take a little longer. For a professional athlete it can be at least a year before they return to sports at a similar level. If you return to sport too soon you have an increased risk of your ACL graft re-tearing.
How much improvement can you expect after an ACL reconstruction surgery?
According to a large study involving 7556 patients undergoing ACL reconstruction, the majority were able to return to sports (81%). Two thirds of all patients were able to return to their pre-injury level of competition, and 55 percent were able to return to elite level competition.13
Knee Injuries In BJJ – How often do they occur?
How commonly knee injuries occur in BJJ is not known. Fortunately the most common injuries in BJJ overall appear to be temporary sprains and strains.14 In a survey of 166 BJJ gyms in the US, lower limb injuries were less common but more severe than upper limb injuries, with 21% of respondents reporting a knee injury.15 Types of injury occurring in training and competition may also differ, as well as between gi and no-gi practitioners, and belt levels.16 In a study of 5022 BJJ competition matches, the overall injury rate was less than 1% with the most commonly injured joint being the elbow due to armbar.17
Summary
To prevent ACL injury, strengthen your quads, hamstrings and warm up properly. If you have torn your ACL and have knee instability, initially try physiotherapy and modify your game. If you still can’t train or compete, then ACL reconstruction may be an excellent solution to your problems.
Background
Dr Alan Cheung is a British Consultant Orthopaedic Surgeon and Director of the International Orthopaedic Clinic, based in Singapore and Shanghai. He has a specialist interest in sports injuries and robotic joint replacement. He is a Ringside Doctor for One Championship and Matchday Doctor for International Rugby events. www.ioc-ortho.com
Follow him on Instagram: @dralancheung or check out his consultancy http://alancheungortho.com.sg
References:
1. Agel J, et al. Collegiate ACL Injury Rates Across 15 Sports: National Collegiate Athletic Association Injury Surveillance System Data Update (2004-2005 Through 2012-2013). Clin J Sport Med 2016; 26:518.
2. Editorial. The female ACL: Why is it more prone to injury? J Orthop. 2016 Jun; 13(2): A1–A4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4805849/
3. Nessler T et al. ACL Injury Prevention: What Does Research Tell Us? Curr Rev Musculoskelet Med. 2017 Sep; 10(3): 281–288. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5577417/
4. Kiapour AM and Murray MM. Basic science of anterior cruciate ligament injury and repair. Bone Joint Res. 2014 Feb; 3(2): 20–31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3922117/
5. Jomha NM et al. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999 Jan;(358):188-93.
6. Mahapatra P et al. Anterior cruciate ligament repair – past, present and future J Exp Orthop. 2018 Dec; 5: 20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6002325/
7. Duffee A et al. Transtibial ACL femoral tunnel preparation increases odds of repeat ipsilateral knee surgery. J Bone Joint Surg Am. 2013 Nov 20;95(22):2035-42
8. Sprowls GR, Robin BN. The Quad Link Technique for an All-Soft-Tissue Quadriceps Graft in Minimally Invasive, All-Inside Anterior Cruciate Ligament Reconstruction. Arthrosc Tech. 2018 Jul 16;7(8):e845-e852.
9. Mayr HO et al. Single-Bundle Versus Double-Bundle Anterior Cruciate Ligament Reconstruction-5-Year Results. Arthroscopy. 2018 Sep;34(9):2647-2653.
10. Manandhar RR et al. Functional outcome of an early anterior cruciate ligament reconstruction in comparison to delayed: Are we waiting in vain? J Clin Orthop Trauma. 2018 Apr-Jun;9(2):163-166.
11. Kay J et al. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018 Jun 6
12. Taketomi S et al. Surgical timing of anterior cruciate ligament reconstruction to prevent associated meniscal and cartilage lesions. J Orthop Sci. 2018 May;23(3):546-551
13. Ardern CL et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014; 48:1543.
14. Stephenson C, Rossheim ME. Brazilian Jiu Jitsu, Judo, and Mixed Martial Arts Injuries Presenting to United States Emergency Departments, 2008-2015. J Prim Prev. 2018 Oct;39(5):421-435.
15. McDonald AR, Murdock FA Jr, McDonald JA, Wolf CJ. Prevalence of Injuries during Brazilian Jiu-Jitsu Training. Sports (Basel). 2017 Jun 12;5(2)
16. Kreiswirth EM at el. Incidence of injury among male Brazilian jiujitsu fighters at the World Jiu-Jitsu No-Gi Championship 2009. J Athl Train. 2014 Jan-Feb;49(1):89-94.
17. Scoggin JF 3rd et al. Assessment of Injuries During Brazilian Jiu-Jitsu Competition. Orthop J Sports Med. 2014 Feb 21;2(2)